Frozen testicular tissue can nonetheless make sperm after 20 years, based on scientists who say it could possibly assist younger most cancers sufferers to later have kids.
Male testis tissue that's cryopreserved could be reimplanted after greater than 20 years and can go on to make viable sperm, based on a brand new examine in rodents within the open-access journal PLOS Biology by Eoin Whelan of the Faculty of Veterinary Drugs on the College of Pennsylvania.
However the work along with colleagues that was revealed on Might 10 discovered that the lengthy delay comes with a price in lowered fertility in comparison with tissue that's solely briefly frozen.
The outcomes might have necessary implications for the therapy of boys with most cancers, for whom chemotherapy could also be preceded by harvesting and freezing of testicular tissue for eventual reimplantation.
The speed of survival for childhood cancers has elevated dramatically within the final a number of a long time, however a critical facet impact of therapy is diminished fertility later in life. A possible therapy could be to reap, freeze, and reimplant testicular tissue, which comprises stem cells, a process which has not too long ago been proven in a macaque mannequin to revive fertility, at the very least after short-term freezing.
However for pre-pubertal boys with most cancers, reimplantation will not be possible for a decade or extra after harvesting, elevating the query of how lengthy frozen spermatogenic stem cells (SSCs) can stay viable.
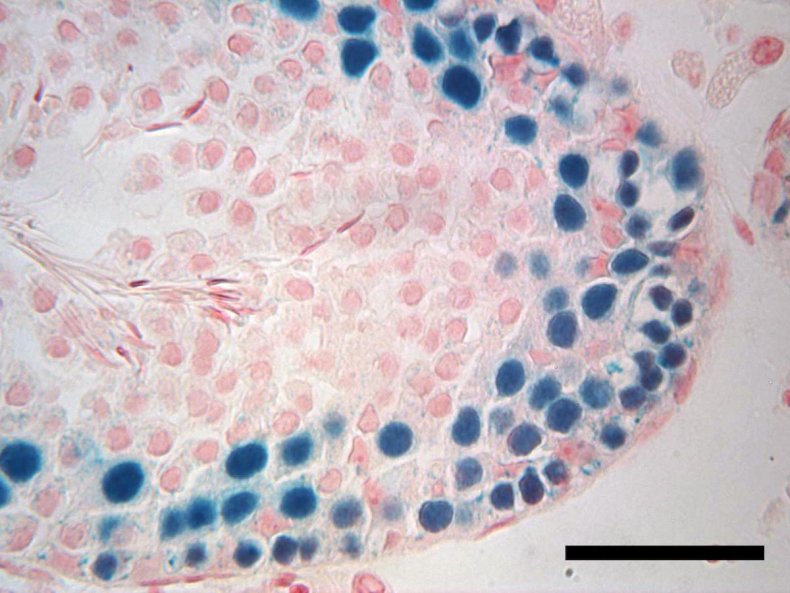
To discover this query, the authors thawed rat SSCs that had been cryopreserved of their laboratory for greater than 23 years, and implanted them in so-called nude mice, which lack an immune response that might in any other case reject the overseas tissue.
They in contrast the power of the long-frozen SSCs to generate viable sperm to SSCs frozen for just a few months, and to freshly harvested SSCs, all from a single rat colony maintained over a number of a long time.
The authors discovered that the long-frozen SSCs had been capable of colonize the mouse testis and generate all the essential cell varieties for profitable sperm manufacturing, however not as robustly as SSCs from both of the extra not too long ago harvested tissue samples. Whereas the long-frozen SSCs had related profiles of gene expression modifications in comparison with the opposite samples, they made fewer elongating spermatids, which go on to kind swimming sperm.
These outcomes have a number of necessary implications.
First, they level out the significance of in situ testing of SSC viability, slightly than counting on biochemical or mobile biomarkers, in figuring out the potential of cryopreserved cells, which can not replicate the precise lack of stem cell potential over time. Second, whereas there presently aren't any protocols that may broaden human SSCs for reimplantation—a requirement for scientific growth of this therapy—such protocols might have to think about time-dependent degradation of viability, assuming human SSCs mimic these of rats. Lastly, and that is the excellent news, viability is under no circumstances misplaced throughout long-term cryopreservation, suggesting that it could be potential to establish and mitigate the important thing drivers of lack of viability, with the intention to enhance the reproductive choices of boys whose childhood cancers are efficiently handled.
Whelan provides, "Our examine confirmed that rat spermatogonial stem cells could be efficiently frozen for over 20 years, transplanted into an infertile recipient animal and regenerate the power to supply sperm, albeit at a lowered price. This might present a technique to recuperate the lack of fertility in prepubertal boys handled for most cancers."

Post a Comment